
Want to Be in a Good Mood? Take Care of Your Guts!
This post is going to be on a more serious note as the topic is a problem for many of us. It’s about mood disorders, depression and other mental issues which many of you have to deal with on an everyday basis. This problem often affects our loved ones.
The basis of mental well-being in patients is, of course, properly personalized treatment and psychological support. But did you know that our gut flora also affects our mood? And that we can shape it so that our mood improves?
Read the post on my blog and find out if probiotics can help you.
Holistic approach to mental issues
Mental health issues should now be treated as a public health problem. Anxiety disorders, depression, mood changes, reduced stress tolerance – each of you certainly knows at least one person struggling with this type of problems. Deterioration in mental state indicates the need to visit a psychiatrist or to work with a psychologist.
However, there is another, equally important issue that is worth considering in terms of mental condition. Namely, when we look at a person in a holistic way, we must take into account that the body affects the psyche, and vice versa.
Our mood, mental well-being, and stress responses largely depend on the state of our digestive tract. Due to the significant connection between the processes in the digestive system and our mental state, the intestines have been called the second brain. And rightly so!
Why do the processes in our digestive tract have such a significant impact on our mental well-being? Because the digestive tract, although it has its own independent nervous system, is also directly related to the brain. I am talking about the vagus nerve, which is the basic element of the entero-cerebral axis. We can imagine this system as a highway, with stimuli flowing in both directions. Formerly it was believed that it is primarily the central nervous system that affects the condition of the digestive tract. This was explained, for example, by abdominal pain or diarrhea appearing at stressful events. The current state of knowledge indicates that the processes taking place in the guts have an equally significant impact on the mental state. Our brain is even “bombarded” every day with a huge amount of impulses coming from the digestive tract. It is not surprising, therefore, that if you want to enjoy a good mood you should definitely take care of your intestines.
An excellent example of this mutual influence is more and more commonly diagnosed irritable bowel syndrome (IBS), described as a disruption of the functioning of the entero-cerebral axis and the intestinal ecosystem. Apparently, it has been often observed that in IBS patients the problem is not only abdominal pain, bloating, diarrhea or constipation. With the severity of these ailments, the patient’s psychological well-being also worsens, sleep quality decreases, and a worse reaction to stress occurs. In some patients mental well-being decreases first, and the next stage is the development of symptoms characteristic of irritable bowel syndrome.
The implementation of effective methods of treatment, probiotic therapy, and a personalized diet which leads to the regulation of the digestive tract, often result in the improvement of mental well-being.
Healthy digestive tract = good mood
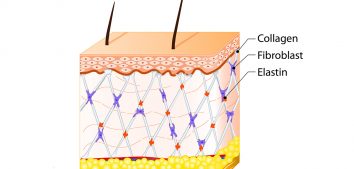
First of all, we must treat the intestine not only as a “tube” for digestion and absorption, but also as a habitat for most (over 70%) immune cells and an incredibly efficient factory that produces a number of metabolites every minute. Whether health-promoting compounds, which favorably affect our body, prevail in this production process depends largely on our microbiota, which comprises about 2 kilograms of bacteria inhabiting the gastrointestinal tract (primarily the large intestine). When we are healthy (i.e. in the state of eubiosis), most of these microorganisms work in our favor. Intestinal bacteria produce B vitamins and K vitamin, they favorably regulate our immune system (which is not only important for efficient infection control, but also plays a significant role in allergic or autoimmune diseases), they also provide a number of enzymes necessary for digestion.
The fact that about 90% of serotonin (colloquially called “the hormone of happiness”) is produced in the intestines, with the participation of intestinal microbiota, is highly important for the proper functioning of the entero-cerebral axis. Another significant issue is the ability of our microbiota to inhibit inflammation in the body by stimulating the production of pro-inflammatory cytokines. At this point, you may wonder what inflammation has to do with mood disorders or depression? Well, a lot! Patients with depression have low levels of inflammation. For this reason, the disease is increasingly being referred to as inflammatory. It is claimed that the effectiveness of antidepressants may also partly result from their anti-inflammatory activity. And it is for a reason…
Scientific research
Links between mood and stress responses and the gastrointestinal tract have been studied for many years. The first hypotheses that schizophrenia may have its source in the digestive tract appeared already at the beginning of the 20th century.
So you can see there must be something about it. What is more, studies have shown that in case of inflammation, which can be caused by intestinal dysbiosis, damage to the intestinal barrier, and the development of adverse reactions to food, the action of HPA axis is affected. Consequently, serotonin is not synthesized from tryptophan (exogenous amino acid), and substances that are toxic to central nervous system structures (e.g. kynurenine) are produced in its place.
Research on laboratory animals has brought a breakthrough. It has been shown that the transfer of intestinal microflora from normal, naturally colonized rats to sterile GF animals (free from bacteria, that is, without intestinal microflora and living in sterile conditions) leads to significant changes in the behavior of these recipients. It has been observed, among others, that animals with transplanted microbiota are more likely to socialize, are more interested in the environment around them, more curious. In other words, they demonstrate positive changes. In subsequent studies, it was observed that feeding mice with broth enriched with probiotics had a positive effect on their response in stressful situations. A second group of animals (the so-called control group) did not receive probiotics. Animals from both groups were exposed to stress-generating situations, such as throwing them into water or placing them in a maze. It turned out that those animals that were given a probiotic came out of the maze faster and also actively tried to leave the water tank. What is important, much fewer behaviors suggesting stress or anxiety were observed during these tests along with lower levels of corticosterone with simultaneous GABA stimulation (the so-called calming brain neurotransmitter).
Psychobiotics
A group of probiotics which has a direct impact on improving mood is becoming more and more popular. They are called psychobiotics. They work by suppressing inflammation, regenerating the intestinal barrier, increasing the production of serotonin in the intestine, and subsequently regulating the functioning of the entero-cerebral axis. Do such supplements help?
Well, the studies carried out so far have shown that such supplementation can improve mental well-being, relieve depression symptoms and bring overall improvement in the quality of life declared by patients. The reason for their use is also recommended due to the fact that the microflora of people with depression and mood disorders is different from that of healthy people. If you suffer from mood problems, you may want to consider assessing your microbiome and implementing personalized probiotic therapy.
In conclusion, it is worth noting that probiotics can neither replace the pharmacotherapy prescribed by a psychiatrist nor psychotherapy, but they are a valuable element of complementary treatment and their use gives really good results for many patients.
Enough of theory for today 🙂 Soon, I will try to show you some simple and practical guidelines on how to take care of the mood from the “intestinal” side.







Comments No Comments
Join the discussion…